Abiomed Recalls the Instructions for Use for Impella Left Sided Blood Pumps due to Perforation Risks
See FDA Recall dated 03/21/2024
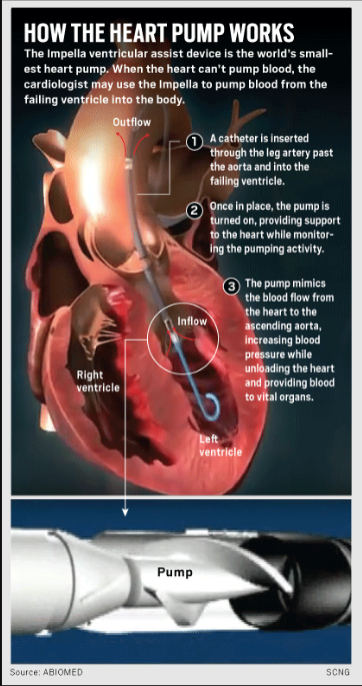
The Impella Left Sided Blood Pump is a mechanical circulatory support device that assists the heart in pumping blood. The device is inserted percutaneously through the femoral artery or the axillary artery. The catheter is moved through the aorta into the left ventricle of the heart.
The pump draws blood from the left ventricle, while the inflow portion of the catheter (placed within the ventricle) captures the blood. The pump then moved the blood through the catheter and sends it into the Aorta, this helps reducing the workload of the left ventricle.
The pump is powered and controlled by an external console that monitors the device and provides option for adjustment.
When Is The Impella Pump Used?
This is a catheter-based device that is used temporarily, for short-term support during high risk procedures or acute heart failure, ensuring adequate blood flow even when the heart is compromised. By reducing the workload of the heart, it allows the myocardium (heart muscle) to rest and recover thereby improving overall heart function.
For example, the Impella pump can be used during Acute Myocardial Infraction, Cardiogenic Shock, or patients with High-Risk PCI
According to the FDA the recall involved about 66,390 that were distributed between 10/10/2021 and 10/10/2023
Why Did The FDA Issue A Recall?
A total of 129 serious injuries have been reported to the FDA, including 49 reports of death. The reason for the recall was because the pump catheter may cut the wall of the left ventricle in the heart. Injuries include:
- Left Ventricle Perforation
- Free Wall Rupture
- Hypertension
- Lack of Blood Flow
- Death
Demographic for Abiomed’s Impella Left Sided Pump
The Abiomed Impella Pump is used for a range of patients, primarily those experiencing severe heart conditions that require temporary mechanical circulatory support. Here are some key demographic details of patients who would typically use the Impella Pump:
- The majority of patients are adults, often middle-aged to elderly, as these age groups are more prone to severe cardiovascular diseases. A significant proportion are older adults, particularly those over 65 years, who are at higher risk of heart failure and coronary artery disease.
- Both men and women use the Impella Pump, though there may be a slightly higher prevalence among men due to a higher incidence of certain types of heart disease in men.
Medical & Clinical Conditions That Can Lead To The Use Of This Device
- Acute Myocardial Infarction (AMI): Patients suffering from severe heart attacks that result in significant heart muscle damage.
- Cardiogenic Shock: Patients who experience a sudden and severe drop in heart function, often following a heart attack.
- High-Risk Percutaneous Coronary Intervention (PCI): Patients undergoing complex or high-risk coronary interventions that require hemodynamic support.
- Heart Failure: Patients with acute decompensated heart failure who need temporary support to maintain cardiac output.
- Emergency Situations: Used in emergency scenarios such as heart attacks or cardiogenic shock where immediate circulatory support is critical.
- Planned High-Risk Procedures: Used preemptively in planned high-risk PCI procedures to ensure stable hemodynamics during the intervention.
- Bridge to Recovery: Occasionally used as a bridge to recovery for patients whose heart function is expected to improve with temporary support.
Geographic Distribution
- Typically used in larger hospitals and medical centers equipped to perform high-risk cardiac procedures and manage advanced heart failure cases.
Socioeconomic Factors
- Insurance Coverage: Patients with comprehensive health insurance or access to advanced healthcare facilities are more likely to receive Impella support.
- Access to Specialized Care: Access to cardiologists and specialized cardiac care centers is a key factor, as these are the settings where Impella devices are most often used.
Here Is A Summary Of Demographic Data For Patients More Likely To Suffer From Acute Myocardial Infarction (AMI), Cardiogenic Shock, High-Risk Percutaneous Coronary Intervention (PCI), Heart Failure, And Heart Attacks:
Acute Myocardial Infarction (AMI) and Heart Attacks
- Age:
- Older Adults: The risk of AMI increases with age, particularly in those over 65 years.
- Middle-Aged Adults: Individuals aged 45-64 are also at significant risk.
- Gender:
- Men: Men have a higher incidence of AMI compared to women, especially before the age of 55.
- Post-Menopausal Women: After menopause, the risk for women increases and becomes more comparable to men.
- Race/Ethnicity:
- African Americans: Higher rates of AMI compared to Caucasians.
- Hispanic and South Asian: Elevated risk compared to non-Hispanic whites due to higher prevalence of risk factors like diabetes.
- Risk Factors:
- Hypertension: Strongly correlated with increased risk.
- Smoking: Major risk factor for AMI.
- Diabetes: Significant risk enhancer.
- Hyperlipidemia: High cholesterol levels contribute to risk.
- Family History: Genetic predisposition plays a role.
Cardiogenic Shock
- Age:
- Older Adults: More common in elderly patients due to higher prevalence of severe coronary artery disease.
- Gender:
- Both Genders: Affects both men and women, though slightly more common in men due to higher incidence of coronary artery disease.
- Clinical Context:
- Post-MI: Most cases occur following an acute myocardial infarction.
- Severe Heart Failure: Advanced heart failure patients are at risk.
High-Risk Percutaneous Coronary Intervention (PCI)
- Age:
- Older Adults: Patients over 65 often require high-risk PCI due to complex coronary anatomy and comorbidities.
- Middle-Aged Adults: Those with significant coronary artery disease requiring intervention.
- Gender:
- Both Genders: Performed on both men and women, but more common in men due to higher prevalence of coronary artery disease.
- Clinical Indications:
- Complex Coronary Artery Disease: Patients with multivessel disease or left main coronary artery disease.
- Previous PCI or CABG: Patients with previous coronary interventions or bypass surgery.
Heart Failure
- Age:
- Older Adults: Most common in individuals over 65 years.
- Middle-Aged Adults: Increasingly diagnosed in those aged 45-64.
- Gender:
- Both Genders: Equally affects men and women, though the cause and progression may differ.
- Race/Ethnicity:
- African Americans: Higher prevalence and more severe forms of heart failure.
- Hispanic and South Asian: Higher risk due to higher rates of diabetes and hypertension.
- Risk Factors:
- Hypertension: Major contributing factor.
- Diabetes: Significantly increases risk.
- Obesity: Strongly associated with heart failure.
- Coronary Artery Disease: Leading cause of heart failure.
Summary of Key Data Points
- Age: Risk for all conditions increases significantly with age, especially in those over 65.
- Gender: Men are more commonly affected by AMI and high-risk PCI; however, women’s risk increases post-menopause.
- Race/Ethnicity: African Americans and certain other ethnic groups have higher prevalence and severity of these conditions.
- Risk Factors: Hypertension, diabetes, smoking, obesity, and hyperlipidemia are major contributors.
Geographic Hot Spots for Cardiovascular Disease
- Southeastern United States:
- States in the Southeast, often referred to as the “Stroke Belt,” including Alabama, Mississippi, Louisiana, Arkansas, and Georgia, have higher rates of heart disease, heart attacks, and heart failure. This region shows significant clustering of high cardiovascular disease prevalence.
- Midwest:
- States like Michigan and Ohio also exhibit higher rates of cardiovascular conditions. Factors contributing to these high rates include higher prevalence of risk factors such as hypertension, diabetes, obesity, and smoking.
- Northeast and New England:
- Parts of the Northeast, including areas in Maine, show elevated rates of chronic heart disease.
- Pacific Northwest:
- Certain areas in the Pacific Northwest, including parts of Washington and Oregon, also demonstrate higher prevalence of cardiovascular conditions.